The story of Zimbabwe’s once legendary health system
It would be an understatement to sum it up as a tragic tale.

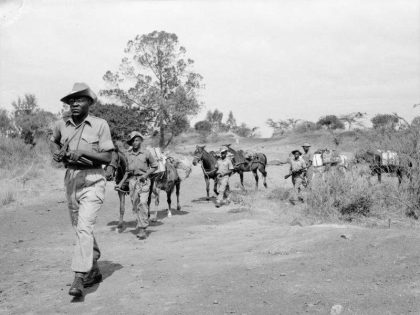
During Zimbabwe’s transition to independence and black majority rule in 1980, the new ruling party, the Zimbabwe African National Union Patriotic Front [(ZANU(PF)], pursued an ambitious vision of modernizing development. Throughout the 1980s, the majority of Zimbabweans gained unprecedented access to education and health care. The government made remarkable progress in the provision of water and sanitation to rural households. According to UNICEF, Zimbabwe’s health sector was, for much of this period, “one of the best in sub-Saharan Africa.” By the 1990s, Zimbabwe could proudly claim a substantial middle class, an educated population, a diversified economy, and a sophisticated public health infrastructure.
In 2008, however, the situation could scarcely look any more different: after a decade-long economic slide, inflation rates – somewhere in the region of 79.6 billion percent – had reached world record-setting levels. Public services had largely disintegrated, while major shortages of basic commodities had been piled on top of political turmoil and violence. The health system was left in extremis. Clinical coverage was inadequate throughout much of the country forcing patients to travel long distances for treatment. At medical facilities, there were critical shortages of essential medicines while frequent electricity outages prevented the use of much hospital machinery. On top of this, a catastrophic cholera outbreak – unprecedented in scale, duration and lethality – was competing for lives with one of the highest HIV rates in the world.
It was thus jarring when President Robert Mugabe, who cynically presided over the collapse of Zimbabwe’s health system, was named as the WHO’s Goodwill Ambassador in the fight against non-communicable diseases at a UN meeting in Uruguay last week. Dr. Tedros Adhanom Ghebreyesushe, the first African director-general of the WHO, motivated this appointment by stating that Mr. Mugabe could use the role “to influence his peers in his region” and described Zimbabwe as “a country that places universal health coverage and health promotion at the center of its policies to provide health care to all.”
Within a matter of hours Mugabe’s appointment was met with a storm of international opprobrium from a dizzying array of human rights groups, journalists, many UN member states and Western politicians. Following a tenure of only a matter of days, Mugabe’s position was rescinded.
Who can say for sure why Dr. Tedros thought this would be a good appointment or, for that matter, why he had not anticipated such an awesome backlash? I might speculate that the appointment was a nod to some misguided conception of pan-Africanism, after all Mugabe remains one of the most articulate defenders of African sovereignty against western political-economic and humanitarian intervention in African affairs. More pertinently though, I question the fervor with which the WHO’s decision was condemned.
It is no secret that Mugabe is portrayed in much western media as the archetypal African tyrant whom liberal proponents of good governance and human rights love to hate. Popular media tropes about Zimbabwe as a pathological and pariah state brought to its knees under the brutal regime of the despot Robert Mugabe provide a compelling but ultimately vacuous account of another failed post-colonial African state. Such discourses are not mere rhetorical flourishes, they belie the formidably complex historical, political and economic processes that brought about Zimbabwe’s crisis in the first place. Furthermore, they provoke belligerent counter-narratives in Zimbabwe and embolden Mugabe’s self-serving anti-imperialist posture. This dynamic augments the many difficulties in the country by creating hostile stand-offs between Mugabe’s government and its erstwhile enemies. As I have written elsewhere, the charged moral condemnation of Mugabe over the 2008 cholera outbreak delayed the humanitarian relief effort to fight the disease, promoted non-engagement between Zimbabwe and western governments, and narrowed down the avenues for third-party diplomatic mediation to ameliorate the crisis. As the well-known idiom goes: when elephants fight, it is the grass that suffers.
Finally, Tedros was not entirely off the mark when he talked of Zimbabwe’s commitment to health equity. Looking beyond the country’s political leadership, there are a multitude of dedicated civil servants, local NGOs, and conscientious healthcare professionals working, often with little remuneration, to deliver medical care in an economically harsh and politically polarized environment. These are the actors who are ensuring there is universal health coverage as enshrined in the country’s 2013 constitution. From this perspective, the story of Zimbabwe’s health system, while undoubtedly a tragic, is nevertheless a hopeful one.